
When you fall pregnant, a new organ grows along with your baby, which supplies your little one with all the important nutrients via the umbilical cord. This is called the “placenta”. The placenta can nestle in various locations in the uterine wall, for example in the anterior or posterior wall, the left or right-side wall and in the upper part of the uterus (in the fundus).
The placenta is not fully formed until the end of the first trimester and then continues to grow until the end of pregnancy. In the first half of pregnancy, the placenta grows faster than the baby, and in the last trimester the reverse.
When the placenta attaches low in the uterus, you’ll hear people referring to it as a low-lying placenta. They’re usually spotted on your routine 20-week ultrasound.
As the uterus grows upwards, the placenta is likely to move away from the cervix. Your midwife will check for this during an extra scan at 32 weeks. If that scan finds your placenta is still low lying, you’ll have another scan at 36 weeks.
At that scan, if the placenta has moved to 2cm or more from the inside of the cervix, then you can choose a vaginal birth. If not, it’s defined as placenta praevia or previa. Only one in 10 women who have a low-lying placenta will develop placenta previa.
Our midwife Katrin Ritter explains the effects of placenta previa during pregnancy and for the birth.

Diagnosis of placenta previa – what does it mean?
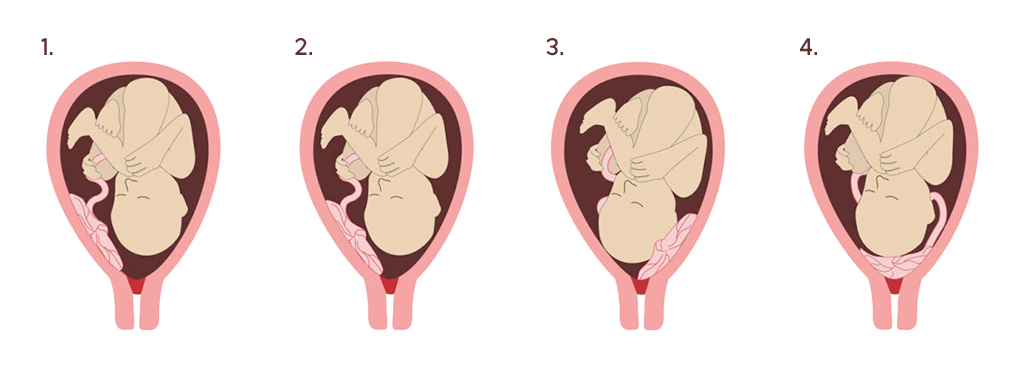
When the placenta covers part or all of the cervix in the last months of pregnancy, it is called placenta previa. Placenta previa can be major or minor: a major placenta previa covers the entire cervix, and a minor placenta previa covers only a part of it. You’ll also hear doctors and midwives calling it ‘anterior’ or ‘posterior’ placenta previa. This depends on whether it is located on the front (anterior) or posterior (back) wall of the uterus.
With an orifice width of 3cm, a distinction is made between:
Deep-seated placenta: The placenta does not reach as far as the inner cervix.
Marginal placenta previa: The placental edge is within 2cm of the inner cervix.
Placenta previa partialis: The placenta has implanted at the bottom of the uterus, over the cervix or close by. The baby can’t be born vaginally.
Complete placenta previa: The placenta covers the inner cervix and thus the entrance to the birth canal completely.
What are the causes of placenta previa?
According to nct.org, it happens in around one in 200 pregnancies. However, it can notionally occur in any pregnancy. It is not yet clear exactly what causes this position, but it is assumed that the fertilised egg has not found a place in the upper half of the uterus for implantation.
The following factors can increase the risk of placenta previa:
- Low implantation of the fertilised egg.
- Abnormalities of the uterine lining, such as fibroids.
- Scarring of the uterine lining (endometrium).
- Abnormalities of the placenta.
- Expecting multiple babies, such as twins.
- Smoking or using cocaine.
- Age of the expectant mother.
How can a placenta previa be diagnosed?
Placenta previa is diagnosed through ultrasound, either during a routine prenatal appointment or after an episode of vaginal bleeding usually in the second half of pregnancy. That’s because this is when the placenta lies in the lower part of the womb, which is stretching as your baby grows. Most cases of placenta previa are diagnosed during a second-trimester ultrasound exam.
Occasionally, placenta previa may be suspected later in pregnancy. This might happen if the baby is in an unusual position, such as bottom first (breech) or lying across the womb (transverse).
What are the symptoms of placenta previa?
Placenta previa does not necessarily have any symptoms – it depends on the severity. However, from about the 20th week of pregnancy, there may be regular, painless bleeding. The blood is fresh and bright red in colour. The bleeding is caused by small injuries to the placenta due to the growth and/or movements of your baby. Please call your maternity unit immediately if you have any bleeding or leaking of fluid (clear or any colour).
Is placenta previa dangerous for mum and baby?
If blood loss is high and frequent, the deep-seated placenta can become dangerous for the expectant mother and her child. This bleeding can occur during pregnancy or only with the onset of labour. In the first case, your baby may have to be delivered via C-section.
Another risk of placenta previa is that it may not detach or detach incompletely after birth, or that it may become attached to the muscles of the uterus.
There is also an increased risk of placental insufficiency (lack of blood supply), premature placental abruption and the rare complication of vasa praevia. This is when your unborn baby’s blood vessels lie unprotected over the cervix and life-threatening bleeding can occur.

What effects does placenta previa have on birth?
If placenta previa is present, a planned caesarean section may be necessary. Most healthcare providers will recommend a C-section between 34 and 37 weeks’ gestation if there are no complications. This prevents you from having contractions or going into labour, as these can cause significant bleeding.
Only in the case of a deep-seated placenta or marginal placenta previa should a vaginal birth be considered in consultation with your doctor. However, for safety reasons, a C-section is often recommended to avoid an emergency caesarean section in case of haemorrhage. Seek advice from your gynaecologist’s practice or your hospital for individual advice on the topic of a deep-seated placenta to discover the best delivery for you and your baby.
We can imagine that some of the explanations may be a little scary. However, it is important that you are well informed and know what it means and what to expect if you are diagnosed with placenta previa. Always seek advice from your doctor or midwife to make an informed decision to deliver your baby safely and keep you safe too!



