
You don’t need to avoid exercise for nine months, unless you have specific medical advice telling you not to do any or to adjust certain movements.
If you exercised before you became pregnant, you can continue to exercise now. The aim should be to keep your current level of fitness rather than trying to reach peak fitness. If you were not regularly active before pregnancy, start off gently and avoid any exercises where you cannot talk without getting out of breath.
Exercise during pregnancy offers many physical and emotional benefits. Physical activity may also help manage some symptoms of pregnancy and make you feel better, knowing you’re doing something good for yourself and your baby.
Exercise during and after pregnancy: We answer the ten most asked questions.
1. Should I exercise during pregnancy?
The NHS guidelines states that the more active and fit you are during pregnancy, the easier it will be for you to adapt to your changing shape and natural weight gain. It will also help you cope during labour and recovery.
If you can, keep up your normal daily physical activity or exercise (sport, running, yoga, dancing, or even walking to the shops and back) for as long as you feel comfortable.
The advantages of exercise during pregnancy include:
Enjoyment.
Increased energy.
Improved fitness.
Reduced back and pelvic pain.
Decreased risk of pregnancy complications such as pre-eclampsia and pregnancy-induced hypertension.
Preparation for the physical demands of labour.
Fewer complications in delivery.
Faster recuperation after labour.
2. What kind of exercise should I do during pregnancy?
Generally, you should be able to hold a conversation as you exercise when pregnant. If you become breathless as you talk, then you’re probably exercising too strenuously. Do not exhaust yourself. You may need to slow down as your pregnancy progresses or if your maternity team advises you to. If in doubt, consult your maternity team.
If you were not active before you got pregnant, do not suddenly take up strenuous exercise. If you start an aerobic exercise programme (such as running, swimming, cycling or aerobics classes). Always tell the instructor that you’re pregnant.
If you have exercised regularly, you can of course continue to do so. However, jogging/running should only be done by trained women.
What are the benefits of pelvic floor exercises?
Your pelvic floor muscles stretch from your pubic bone at the front of your pelvis to the base of your spine at the back. They help with posture and support your bowel, womb, and bladder. It is important to exercise your pelvic floor muscles during and after pregnancy to keep them strong. This can lower the chance of leaking urine when you cough or sneeze (stress incontinence).
Doing pelvic floor exercises regularly can also help to reduce the length of labour. You can exercise them at any time of day, wherever you are, without anybody knowing. You could try doing them every time you put the kettle on or have a drink.
3. What should my heart rate be during exercise?
We do not recommend the pulse method, as the load pulse is not meaningful in pregnancy. The reason is that the blood vessels dilate during pregnancy, but the blood volume does not increase to the same extent. This leads to a decrease in the exercise pulse and an increase in the resting pulse rate. For this reason, we recommend paying less attention to your pulse and more to your body and how you feel.
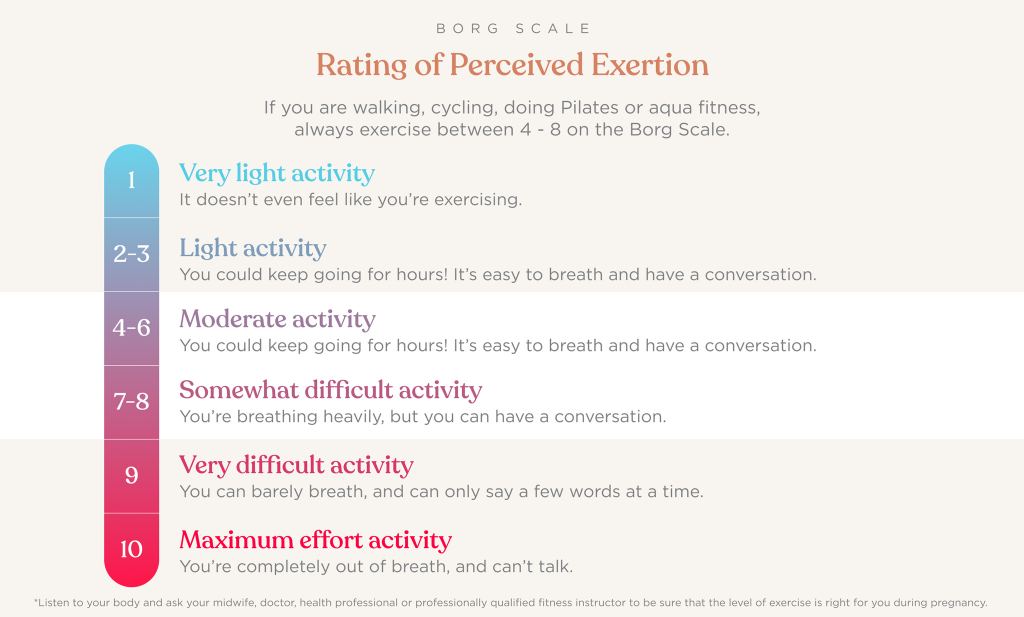
It may help to use the Borg Scale of Rate of Perceived Exertion (see below).
Make sure that you always stay in a medium range between 4 and 8 when exercising during pregnancy. This means exercising in the moderate range (5-6) if you feel like you are climbing stairs or riding a bike fast and exercising intensely if you can still talk while exercising. It is important that you do not go into the extreme effort range (more than 8).
4. How often should I exercise during pregnancy?
The NHS recommend keeping active daily – 30 minutes of walking each day can be enough, but if you cannot manage that, any amount is better than nothing. Remember to always warm up before your workout and cool down afterwards and drink plenty of water to stay hydrated. If you go to exercise classes, make sure your fitness instructor is Pre and Postnatal qualified and knows that you’re pregnant, as well as how many weeks pregnant you are.
5. What about weights, strength training and CrossFit?
With your healthcare provider’s approval and guidance from a qualified fitness professional, weightlifting is a great pregnancy exercise and strength-training practice. Lifting weights while pregnant can strengthen your abdominal and back muscles, increase your stamina for labour and delivery, and even boost your mood.
For CrossFit, women who are pregnant can safely train with CrossFit. However, like with any exercise regimen, there are always safety considerations. With pregnant women, there are some specific things to consider: Have you done CrossFit before? Are you experiencing a normal or a high-risk pregnancy? Which movements and Olympic lifting loads feel good? Which do not? How is your body changing as the pregnancy progresses and the baby develops?
6. Is abdominal muscle training ok?
Training the abdomen, back and pelvic floor is particularly important during pregnancy. However, the straight abdominal muscles should no longer be trained in isolation from the 20th week of pregnancy at the latest. You can strengthen the straight abdominal muscles by doing static exercises where the muscle length remains constant, e.g., balance exercises instead of crunches. Training the oblique abdominal muscles, on the other hand, is highly recommended. With all exercises, however, always make sure you do them in a controlled and careful manner. If in doubt, speak to a qualified pre and postnatal trainer.
7. When can you start exercising after giving birth?
The standard NHS procedure is to offer a postnatal check between six and eight weeks after the birth, during which your doctor should take your blood pressure, find out how you’ve healed and so on. Before you start exercising again, you should have completed postnatal retraining. In the case of a vaginal birth, you can start about 6 to 8 weeks after the birth. In the postpartum period, only light regressive, and metabolic exercises, as well as exercises against thrombosis, are recommended. During this time, you should rest frequently and give your body time to heal and recover. If you want to slowly increase your step count, go for a daily walk or do light leg and arm exercises, which will not strain your pelvic floor and abdominal muscles and will help you to recover.
8. What about C-sections & challenging labours?
If you’ve had a C-section or a complicated pregnancy, you’ll need to get advice from your GP before doing any kind of postnatal exercise. Your GP will look at your alignment, joint movement, breathing and muscle strength, check your stomach for diastasis recti (a postpartum abdominal condition) and assess your pelvic floor. From there, they’ll devise a bespoke rehab plan.
9. When can my body bear its full weight again?
Every body is different. The pelvic floor is usually only fully resilient again after 10 months. It is therefore advisable to do sports that do not put too much strain on the pelvic floor until then. The pelvic floor will only be able to bear its full weight again after complete involution, i.e., after about 10 months and when mum has finished breast/chest feeding, provided there are no complications. Please always listen to your body and seek advice if you are in doubt.

Exercise after birth: This is what your return to exercise may look like:
Postpartum (4th week to max. 8th week) after birth: initially prone positioning on pillows, postpartum gymnastics, abdominal massage. Later, moderate everyday activities, such as climbing stairs, going for walks, abstaining from sports other than postnatal classes, pelvic floor training.
1.5 to 2 months after the birth: 6 to 8 weeks after the birth you can start with your postnatal regression. This usually lasts 8 to 10 weeks. If you are attending postnatal group classes, you can always repeat these exercises at home to rebuild your strength and recovery.
4 – 5 months after birth: Once you have successfully completed your regression, you can start gentle sports such as swimming, aqua fitness, walking, cycling, cross trainer, stepper, Pilates, yoga, baby swimming or similar.
6 months after birth: Now other sports such as running, trampolining, CrossFit, weightlifting, martial arts, or athletics are allowed.
10: How to Ease into an Exercise Routine After Birth?
There are many postnatal exercise classes available to strengthen your muscles and support you and your baby during your recovery journey. Here are a few ideas to consider:
Join a postnatal exercise class.
Lots of postnatal classes allow you do the class with your little one. Some include you wearing your baby in a baby carrier, or your baby stays in their pram or buggy as part of the workout. Breathable baby carriers like our Aerloom are perfect for shared activities or a little sport. Made from FormatKnit, the ultra-lightweight carrier hugs your body like a second skin and allows you to walk or exercise with your baby without sweating excessively due to physical closeness.



Build activities into your day.
Use the stairs instead of the lift or, for short journeys, use your stroller such as our Metro+ Deluxe and walk instead of taking the car.
Push the pram or buggy briskly.
Remember to keep your arms bent and your back straight. Make sure the handles are at the right height for you – your elbows should be bent at right angles. Walking is great exercise, so try to get out as much as you can.
Try swimming.
It’s good exercise and relaxing, but you’ll need to wait until 7 days after your postnatal bleeding has stopped. If you take your baby with you, try to have someone else there to mind your little one so you have a chance to swim too!
Borrow, buy, or watch exercise videos online.
This is a good way to workout at home. You could get a friend or your older children to join in too!



