Hip dysplasia baby: detect early, treat correctly.
"The main thing is for the baby to be healthy" is so often said when parents to be are asked the preferred gender for the expected baby.
However, not everything always goes smoothly with the physical development of your baby in the womb. It is not at all uncommon - in about 2-4% percent of newborns - for congenital or acquired hip dysplasia to develop. If this occurs, baby then suffers from a malformation/maturation disorder of the acetabulum (socket).
Our expert Stephanie Schmitz, functional senior physician for paediatric orthopaedics at the Asklepios Klinik Bad Abbach, the teaching hospital of the University of Regensburg, explains how early screening and modern therapies can help with this diagnosis and avoid late consequences.
How does hip dysplasia develop?
In Central Europe, acquired hip dysplasia occurs at a rate of 2%- 4%, with girls being affected up to five times more frequently. The risk of developing hip dysplasia increases if there is a family history of hip dysplasia or if there is confinement in the womb due to low amniotic fluid, breech position or multiple pregnancies. Hip luxation, a particularly severe form of hip dysplasia, occurs much less frequently, at 0.5% -1%.
How do you recognise hip dysplasia in a baby?
Your baby's hips will be checked as part of the newborn physical screening examination within 72 hours of being born, and again at 6 to 8 weeks of age.
The examination involves gently moving your baby's hip joints to check if there are any problems. It should not cause them any discomfort.
If a doctor, midwife or nurse thinks your baby's hip feels unstable, they should have an ultrasound scan of their hip between 4 and 6 weeks old.
Babies should also have an ultrasound scan of their hip between 4 and 6 weeks old if:
There have been childhood hip problems in your family.
Your baby was born in the breech position (feet or bottom downwards) after 28 weeks of pregnancy
If you have had twins or multiples and 1 of the babies was in the breech position, each baby should have an ultrasound scan of their hips by the time they're 4 to 6 weeks old.
Sometimes a baby's hip stabilises on its own before the scan is due, but they should still be checked to make sure.
Source NHS website.
Can I recognise hip dysplasia in my child myself?
That is certainly possible. Usually, a slightly shortened leg is seen on the side of the dysplasia. The hip cannot be spread sufficiently compared to the opposite side. Anyone who discovers asymmetrical buttock folds in their baby should have this clarified in a paediatrician's practice.
What should I do if my baby has hip dysplasia?
In a milder form of hip dysplasia, nothing needs to be done for the first six weeks from a medical point of view. However, in order to influence the maturation process, positioning the hip in a splayed and flexed position is beneficial. We recommend carrying you baby in a wrap or an ergonomic newborn baby carrier, as the position of the hips is optimal.
During ergonomic carrying, the heads of the hips are pressed into the centre of the hip socket and thus receive a stimulus to mature. Tightly wrapping the hip joints and legs should not be done under any circumstances, as this creates exactly the opposite movement of the hips and can lead to a worsening of the hip situation. However allowing the hips to move freely or in a squat-splay position, can be carried out (e.g. with the Ergobaby sleeping bag). This should be discussed with your paediatrician beforehand.
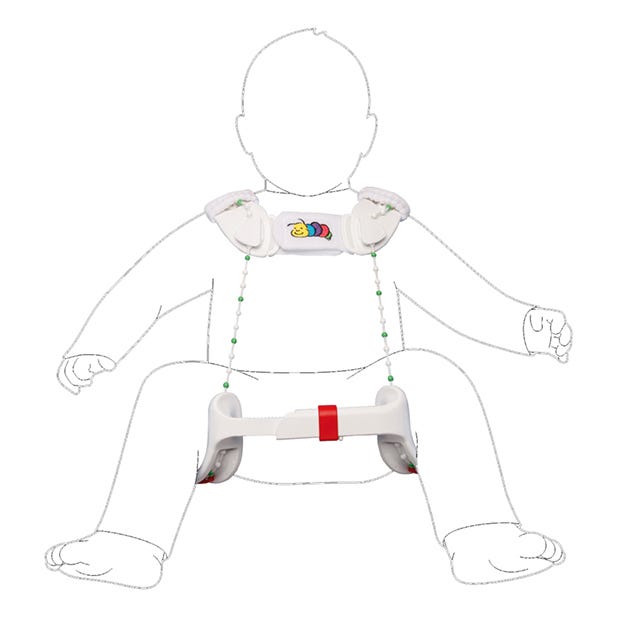
If a more severe form of hip dysplasia is detected during hip screening, there are various treatment options. If the femoral head is still in the acetabulum (socket) and the acetabular roof is still too steep, i.e. it is still not fully extended, one would, for example, start treatment with a Tübingen hip flexion splint. This is a splint that is worn over clothing for at least 23 hours a day and is only removed for changing or bathing. With the help of the splint, the femoral heads are centred in the acetabulum by spreading them out and keeping them bent, thus providing the stimulus for the acetabulum to mature again. The development can be monitored by regular ultrasound checks. The splint is worn until post-maturation is achieved. On average, this takes about 6 to 8 weeks. Checks are only carried out when the child can walk independently.
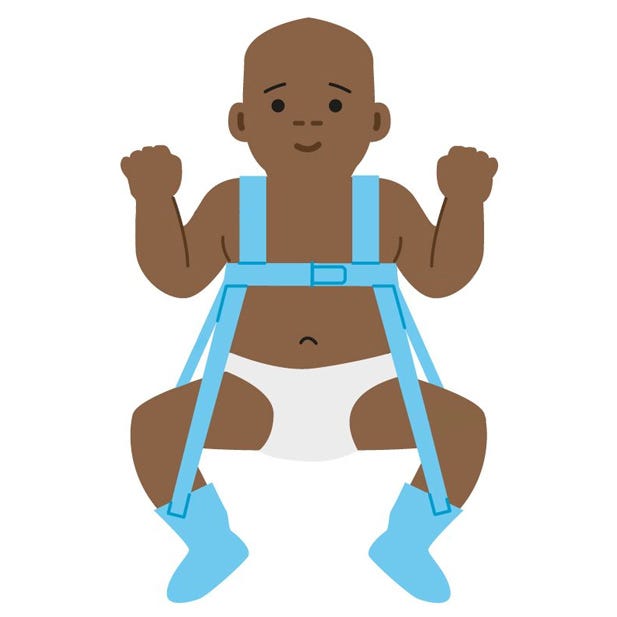
If the femoral head already has a tendency to move out of the acetabulum, a so-called Pavlik harness would be prescribed, which is worn on the skin around the clock and may not be removed by the parents. This therapy is also monitored by regular ultrasound checks. However, the duration of treatment is usually much longer. If the femoral head has already completely dislocated from the acetabulum, the application of a pelvic bone cast is always necessary; in the worst case, surgical intervention may even be necessary.
Can I wear my baby in baby carrier despite the orthosis/orthopaedic device?
Yes, absolutely. Since the splint/support simulates exactly the post-maturation position of the hips, it does not hinder carrying in an ergonomic baby carrier. However, first seek advice from a babywearing specialist to find out which carrier is the most comfortable solution for baby and you. This should always be discussed with the therapist or doctor before your baby is carried.
Who treats hip dysplasia?
For children with a family history of hip dysplasia or delivery from a breech presentation, the first ultrasound should be performed in the clinic by the paediatrician. If a higher degree of dysplasia is already detected, further treatment by a specialist paediatric orthopaedic practice is necessary. In case of abnormalities, referral to paediatric orthopaedics would be made in order to initiate further treatment.
Is hip dysplasia curable?
If hip dysplasia is recognised in time and treated appropriately, consequential damage can be prevented.
We hope that you are reassured and know that there is a lot that can be done for hip dysplasia. Carrying your child is an important aid that supports maturation and healthy development in the best possible way.